Breast cancer screening in France
Radiologist Dr Bruno Scheffer believes that Real-time Tissue Elastography should be routinely used
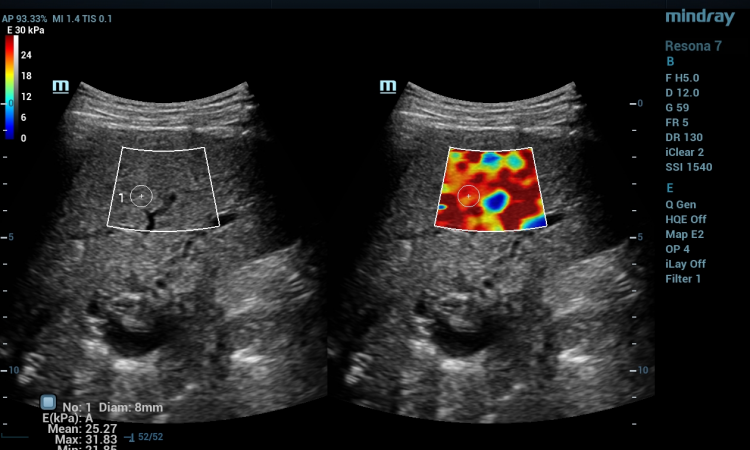
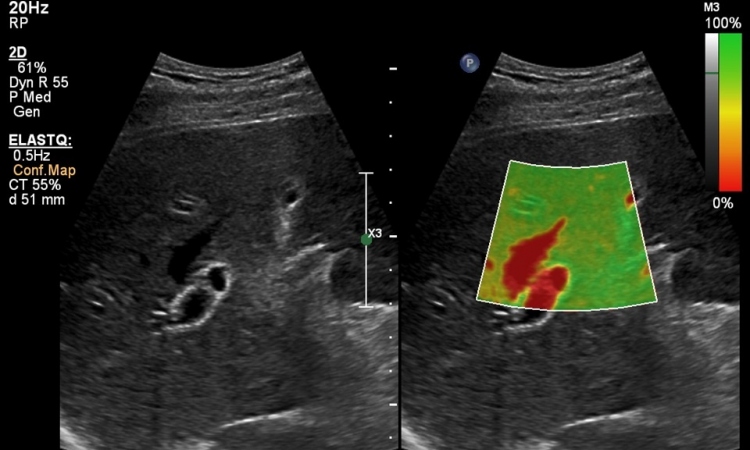
Real-time Tissue Elastography, an ultrasound procedure that uses colour to differentiate clearly and unambiguously between malignant, hardened tissue and flexible, benign tissue could be the addition needed to have really effective breast cancer screening, according to independent radiologist, and specialist in Real-time Tissue Elastography Dr Bruno Scheffer from Nantes, France.

The underlying principle of Real-time Tissue Elastography utilises the process of tissue compression (stressing force) to produce strain (displacement in response to stress) within the tissue; strain is larger in normal, softer tissues and smaller in hard tissues altered by disease. By measuring the strain induced by tissue compression it is possible to estimate tissue stiffness. When a discrete hard non-homogeneity, such as a tumour, is present within a region of soft tissue, it can be unequivocally identified by its stiffness. The technique is so sensitive that Dr Scheffer has found a tumour of only 2 mm. A huge difference from 20 years ago, when he first began to practice, when routinely the tumours discovered were between 25 and 30 mm and significantly smaller than the <10 mm of 90% of tumours discovered today.
Why is this important in breast cancer screening? To be truly effective a breast screening programme has to be sensitive and reproducible (and also cost-effective) enough to detect the lesions as early as possible, to treat the cancer before it becomes too large and has diffused to the ganglia.
France’s nationwide breast cancer screening programme aims to provide a mammogram, every two years, for at least 80% of women aged 50 to 74. To have significant health benefit, surveys have shown that, to reduce breast cancer mortality by 20-30%, at least 70% of the healthy population aged over 50 should be screened. Figures show five breast cancers are detected for every 1,000 mammograms, with 42,000 new cases diagnosed annually in France perhaps current procedures could be improved?
The mammogram is the starting point for any screening procedure, says Dr Scheffer. ‘Looking at a mammograph is the first signal to an experienced radiologist that there is a potential problem and, of course, it helps to refine and localise our search. It is the next steps that are more controversial. In the case of a suspect mammograph, B-mode ultrasound is used to further investigate and characterise the area of risk, then this is followed by the invasive technique of biopsy, either fine-needle, micro- or macro-, to diagnose the suspected tissue by histopathology. B-mode ultrasound following a normal mammography may also highlight areas of suspicion. Without positive guidance from mammography it is often difficult to decide which areas are most likely to be lesions resulting in multiple biopsies being performed for subsequent histopathological confirmation.’
Finding that he was performing too many biopsies encouraged him to investigate other techniques that could reliably remove the need for biopsy while not increasing the rate of false negatives. Ideally the technique would also be sensitive enough to capture lesions that he would have overlooked using traditional B-mode. He has found that Real-time Tissue Elastography fulfils all these requirements and has used it routinely in his practice for the past three years.
Using elastography which is performed in real-time, at the point when ultrasound has confirmed the presence of a suspect mass, can provide a rapid response; an initial examination can be performed in as few as 30 seconds. Patients with benign conditions can be promptly reassured and discharged, removing the healthcare and psychological costs of surgical biopsy or repeated follow-up.
With the decisional, work-flow chart Dr Scheffer has developed for use with the Hitachi HI-RTE System he can improve specificity in the characterisation of non-palpable breast lesions and the management of BI-RADS 3, 4 and 5 nodules, leading to a decrease in false-positives and short term follow-up rates.
Real-time Tissue Elastography is validated as a technique, says Dr Scheffer, there are over 2,500 published cases from Europe alone. ‘With elastography I can reduce the number of biopsies performed, reassure patients and importantly eliminate false negatives. I feel that real-time elastography is missing from current screening practice and its inclusion in the diagnosis of breast cancer would ultimately be better prognostically for patients and also cost-effective for healthcare providers.’
Report: Jane MacDougall
01.07.2009