Elastosonography and the detection of breast carcinomas
Professor Friedrich Degenhardt (right), Head of the Gynaecology Clinic at Franziskus Hospital, Bielefeld and the Cooperative Breast Centre Bielefeld-Herford, Germany, is using elastosonography to examine breast carcinomas. We asked him to outline present finding as to its value, future potential, and the current value of ultrasound in breast cancer detection.
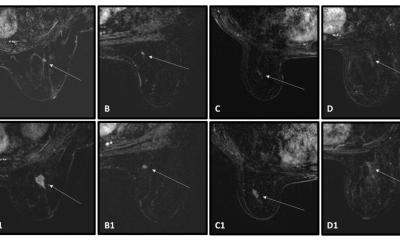
‘We are currently carrying out elastosonography examinations to achieve a differentiation between benign and malignant growths, to find out a cut-off which gives us the chance to find out more about the nature of a tumour, an assessment of malignancy i.e. the histological result of a breast tumour,’ Professor Friedrich Degenhardt explained. ‘We have just finished a doctorate on more than 200 cases and were able to draw good conclusions. As this doctorate is not yet fully evaluated, I can’t give more details. However, it will be interesting to see whether we will actually achieve a closer prediction of tumours with this additional gray-scale imaging.
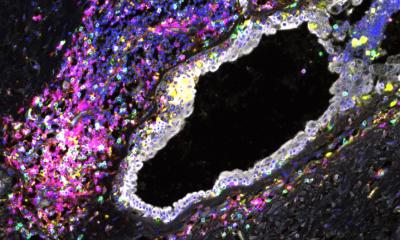
‘Using the new Hitachi Elastosonography System, first we are able to show differentiated images of these tumours. Then the small boxes are superimposed on the tumour tissue. We then superimpose the same boxes on tissue that does not appear to have any pathological characteristics based on the ultrasound image. The density value for what we believe to be normal breast tissue is then compared with the density value of the tissue which appears pathological. Based on this density ratio we are able to achieve better conclusions about the tumour tissue.’
Asked whether elastosonography become an established procedure in the future, Prof Degenhardt said this is primarily a health-political question. ‘It is definitely of great help in the differentiation between benign and malignant tumours. So, if we say that we only want to operate on those patients with a malignant result, then elastosonography is a good basis for such a decision.’ However, he added: ‘Healthcare politics is currently leaning towards mammography screening. But there are an increasing number of examinations that show that ultrasound could be equally, or in some cases even more effective than mammography. There are now special procedures in ultrasound scanning technology that allow us to depict a tumour slice by slice, almost as with MRI technology. I imagine that we could more or less match MRI quality and possibly limit the use of MRI for very specific areas.’
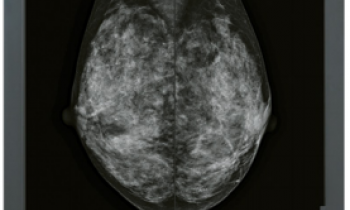
Although there are currently three procedures – mammography, MRI and ultrasound – healthcare politics currently only favours mammography, he pointed out. ‘For the first time, the new S-3 guidelines recommend ultrasound for women, up to the age of 40, who have a lump in their breast. For women between 50 and 69, mammography is the recommended procedure. However, for women with a high breast tissue density mammography does not always deliver good results. This means that breasts in categories ACR3 and ACR4 (ACR = American College of Radiology) ultrasound has to be carried out additionally to confirm results.
‘
The S-3 guidelines contain directives about the detection of tumours, whether they are benign or malignant and how to treat them. As I said, younger women, around the age of 50, or women who take hormones, often have very dense glandular breast tissue. It has transpired in recent years that a proportion of carcinoma within this group has not been detected. This is why ultrasound should be used here. If necessary, elastosonography or gray-scale imaging can also be used, which depends on what type of equipment doctors are using. If the appropriate equipment is available elastosonography can be carried out. The procedure of gray-scale imaging is currently not very wide-spread, it is still a field of investigation.
‘The outlook is definitely very promising. I should add that ultrasound is currently still a little underrepresented in breast diagnostics, and something has to change. Maybe this is because, with mammography, imaging can be carried out by radiographers, whilst, in Germany, ultrasound has to be carried out by doctors, which means we cannot offer ultrasound on a large scale because we do not currently have the required number of doctors trained in this area.’
28.10.2008