Muslims and healthcare in the United Kingdom
By Brenda Marsh
Britain is a primarily Christian country. It is also home to people with various religious beliefs who have migrated here from many parts of the world, or are British born. In a 2001 census, 72% of the population identified itself as Christian.
The next biggest religious faith was Muslim (2.7%), followed by Hindu (1.0%), Sikh (0.6%), Jewish (0.5%) and Buddhist (0.3%), and the rest followed other religions, had no faith, or stated none for the census.
In terms of numbers, seven in every ten people in Britain claimed to be Christian; the Muslim population equates to 1.6 million people; Hindu to 599,000; Sikh to 336,000, Jews to 267,000, and so on.
In August, the statistical research body Eurostat released projections that suggest that the current UK population of around 61 million could increase steadily to about 77 million by 2060. Healthcare and social care may account for a huge increase in numbers – particularly of old people.
These figures are not just of interest; they also reflect Britain’s changing way of life.
With its long history of Empire and Commonwealth, Britain has long prided itself in welcoming and assimilating immigrants. However, change is not easily accepted by all.
Thus, when Muslim groups began to request that various religious needs should be met within the National Health Service (NHS) these have been met with a mixture of willingness and generosity but also consternation. The situation
is often controversial, not least because so many hospital practices are challenged.
Medical students and staff dress: Although Muslim women medical students were allowed to wear
the full-face veil for lectures and on the campus, Birmingham University School of Medicine banned this in hospital clinical areas and in GP surgeries, on the grounds that it could prevent good communication between them and their colleagues – as well as patients. It was said that regulation surgical masks provide adequate face covering in the operating theatres. Headscarves worn as part of religious observance were to be allowed.
A recent Department of Health guidance stipulates that all doctors must be ‘bare below the elbow’, to help prevent infections. Various hospitals have received objections from Muslim women trainees who do not wish to remove arm coverings in the operating theatre and to roll up their sleeves when hand washing. In terms of hygiene, this is vital. However, it is a problem for some Muslims: one university hospital reported that some students said they would rather give up their studies than bare their arms.
Nonetheless, the Islamic Medical Association insisted: ‘No practising Muslim woman – doctor, medical student, nurse or patient – should be forced to bare her arms below the elbow.’ The problem continues.
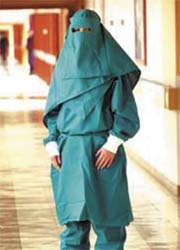
Patients’ gowns: In 2005, a hospital gown, called the ‘inter-faith gown’, was designed to comply with rules on women’s dress, in Muslim, Hindu, Orthodox Jewish and Rastafarian faiths.
Made by the UK company Interweave Textiles (www.interweavetextiles.com), one of the biggest suppliers of textiles to healthcare and contract markets, these jade green polycotton garments come in five pieces, which include trousers and a choice of head pieces, to cover the head, neck and body, leaving only a gap for a patient’s eyes. They also
have elasticated cuffs to ensure women’s arms are not revealed.
Inspired by Karen Jacob, linen services manager at Lancashire Teaching Hospitals, the gowns were tested for a 12-month period at Lancashire Teaching Hospitals. ‘The use of the gown at our Trust produced some very positive feedback from patients,’ she said.
A Lancashire Teaching Hospitals NHS Trust spokesperson said the gown was introduced ‘… because some ladies simply felt they could not wear the normal gown which, as we know, can show parts of us we do not want on show. We have had examples of people not showing up for operations. This can only help.’
In November 2006, the inter-faith gowns went on general sale, costing about £16 per set.
Gender of patients and doctors: The preference among Muslims is to be seen by same sex doctors. However, if no female doctor is available, some women may agree to be seen as long as another woman (e.g. a nurse) is present. Others may refuse to be seen. Mixed wards also cause stress to female Muslims, but this is also disturbing to women patients of any faith.
Beds to face Mecca: Last December, the Mid-Yorkshire NHS Trust proposed that Muslim patients’ beds should be turned to face towards Mecca five times a day. Running water should also be provided for these patients to wash before and after their prayers, and for many other purposes.
This was first implemented in the Dewsbury and District Hospital, Yorkshire, where there is a large Muslim population. A spokeswoman for the Mid Yorkshire Trust said: ‘This is all part of our holistic approach to treating patients of all faiths. Where it is safe and practical we will move the beds of seriously ill patients so that they face towards Mecca five times a day, should a patient request it. We are keen to accommodate all faiths, for example if a patient is Roman Catholic then we would try and ensure they can receive Holy Communion.’
However, critics of the ruling said it would be far better to create Muslim-only wards, with all beds facing Mecca, than to burden overworked nurses with this extra task.
Religion: British hospitals generally house Christian chapels and many have multi-faith prayer rooms.
The Ashford and St. Peter’s Hospitals, serving a diverse population of over 400,000 people, have provided a Christian chapel and improvised arrangements for other faiths. Recently, however, a Multi-faith Centre was opened at St. Peter’s, and a similar project is planned for Ashford.
The Centre comprises the existing Chapel, Multi-faith Prayer Room, Quiet Room and Ablutions Room for ritual washing before prayer, and also provides a shoe rack for footwear. The ample Prayer Room floor has a simple compass design. Secure storage space is provided for sacred texts and religious artefacts.
‘Our vision was to develop the Chapel area to provide more fitting facilities for all who wish to spend time in quiet, reflection, meditation or prayer,’ explained Judith Allford, Head of Pastoral Care for both hospitals. The new double doors, set with decorative glass, link the Multi-faith Prayer Room to the Chapel. These, she explained, have both a practical and symbolic purpose. ‘Practically, they offer the option to extend the space in both the Prayer Room and the Chapel when the need arises. Symbolically, they represent the welcome and hospitality which it is our desire to offer to one another across our different faith traditions.’
Representatives of Christian, Muslim, Hindu, Jewish and Buddhist faiths attended its July opening. Candles were lit and sacred texts and other religious artefacts were donated by the religious groups.
Drugs: There is concern that, although Muslims must avoid porcine and alcohol derived drugs, possibly objectionable drugs may not be labelled as such, nor advice given on alternatives.
Catering: Some outside catering services in Britain can provide not only halal food, but also the necessary equipment for their hygienic handling.
Ramadan and Hajj: Recognition of their importance has been advised, for example not to book hospital appointments for Muslim patients during these events.
During Ramadan, the holiest of Islam’s four holy months, eating, drinking and sexual relations are forbidden in daylight hours. Last year, the Scottish Executive and the Scottish NHS issued a guidance
that, during Ramadan, ‘consideration’ should be shown to Muslim colleagues and patients. Food should not be eaten in front of them, and food trolleys kept away.
Are separate faith-based hospitals the answer?
Aziz Sheikh, professor of primary care research and development in the Division of Community Health Sciences, University of Edinburgh, and principal investigator on a Scottish Executive supported grant to investigate the end-of-life care needs of South Asian Sikhs and Muslims in Scotland, advocates that doctors and health policy makers should realise their needs and provide specific services for them.
It is even suggested that faith-based hospitals may improve the well-being of Muslim patients. (Moscow’s first private clinic based on Sharia law opened last year. Among other things it observes gender differences, supplying female or male specialists according to a patient’s gender. The doctors show only their hands; female doctors wear headscarves or hijabs. In the prayer room a screen separates men from women. Halal food is served.)
In Britain, although male infant circumcision is not approved by the National Institute of Clinical Excellence (NICE), Professor Sheikh believes that male infant circumcision should be available throughout the NHS. A few Trusts do provide this service, but most Muslim parents must resort to poorly regulated operators, sometimes unhygienic and dangerous.
Conclusion: There is a laudable commitment to prevent racism or religious prejudice in all public services. Certainly, small advances have been made, but with so many issues involved, the way forward is by no means straightforward.
* Should Muslims have faith based health services? BMJ 2007; 334:74 (13/1/08), doi:10.1136/bmj.39072.
347720.68
01.09.2008





