Searching Brain Pathways for Clues on Autism
Research findings on a global autism epidemic from the Children's Hospital of Philadelphia
Timothy Roberts, PhD, works in the middle of an epidemic. In the 20 years the researcher has studied autism, the diagnosis rate among children in the United States has risen from one in 1,000 to one in 88. No one is sure of the cause, how to prevent it, or how to treat it.


Some of the answers may come at The Children’s Hospital of Philadelphia (CHOP), where Roberts and his peers are conducting cutting-edge research on the often debilitating spectrum of brain disorders, aided by Siemens scanning technology. There, leaders in the field of autism research are looking for clues in the wiring of the brain that they hope will shed light on one of modern medicine’s darkest secrets: the cause of – and possible cure for – autism.
Wide Spectrum of Autism Symptoms
Autism, a set of brain disorders that affect a child’s social and behavioral development, is typically diagnosed when a child is between two and five years old. Symptoms range across a wide spectrum, from severe communication disabilities and repetitive movements, to social awkwardness. Boys are about five times more likely to be diagnosed with autism than girls, according to a study by the Centers for Disease Control and Prevention. That same study found that white children are slightly more likely to develop autism than black and Hispanic children.
Children in other developed countries have rates similar to that of the USA, with some variation for cultural differences in what behaviors are within the autism spectrum, says Roberts, who is Vice Chair of Research in the Department of Radiology and part of the Center for Autism Research at CHOP. “These children and young adults have difficulty maintaining social interactions,” Roberts says. “Sometimes they don’t get social cues; sometimes they don’t feel comfortable in social situations. That’s probably the most devastating area.”
Also devastating is the rising number of diagnoses. “It does seem like an epidemic,” Roberts says. “In fairness, awareness in 2012 is much greater than it was five years ago, and certainly greater than 10 years ago. Many cases were being missed in the past. Today, parents are more informed, and primary physicians are more informed.” In addition, the diagnostic category has been broadened beyond the “classic autism” of repetitive movements and severe communication problems. “It’s likely you’re going to get more cases, just because you have a broader definition,”
Roberts says. “And yet, those two factors alone cannot account for the prevalence figure of one in 88 [when it used to be one in 1,000],” Roberts says. “There is a real biological basis to the growth as well.”
Many Disorders, Few Answers
The nature of that biological basis continues to be a daunting challenge for researchers. What we know is that autism results from a complex interaction of genetics and environment. “It’s not a single gene,” Roberts explained. “There maybe 10 or more genes that have to interact, and even then, they may require an environmental trigger. So you need the genetic predisposition and the environmental trigger.”
Complicating the research is the fact that autism is an umbrella term covering various disorders with different behavioral manifestations and, likely, causes. In some rare cases, autistic children are able to accomplish mental feats that few “normal” people can. “It’s not inconceivable that some will function better, in some niche way,” Roberts says. “They may have [brain] connections that may be absolutely optimal for remembering 24-digit numbers, something the rest of us can’t do.”
A recent study published in Intelligence magazine found that eight prodigies in music, art, and math scored high in autistic traits, most notably a stunning attention to detail. “It’s all a question of degree,” Roberts says. “Autism is a big mystery. It’s a very heterogeneous disorder.”
Searching for Commonalities
While the behaviors of autistic children are different, Roberts theorizes that there are commonalities deep in the brain. “There might be a fundamental enough level of abnormal conductivity that there will be common features that unite these children,” he explains. Find that commonality, and doctors can begin the search for treatments that go beyond the behavioral treatment of today.
Roberts’ research looks for those commonalities in the wiring of the brain, particularly the pathways for sound. He says the brains of eight of every 10 autistic children respond to sound about one-hundredth of a second later than the brains of non-autistic children. In a casual conversation, autistic children’s brains may be ten words behind. “These delays add up and cascade,” Roberts says. “Suddenly, conversations become complex.” Not only does the research indicate a possible reason for the communication problems of many autistic children, but it could be used as a biomarker to diagnose autism at an earlier age. That’s important, because behavioral therapies for autism are more effective the earlier they begin, Roberts says.
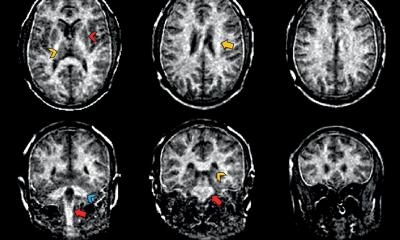
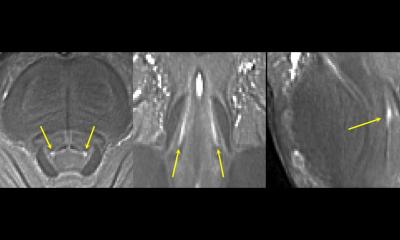
To help with diagnosis, researchers at CHOP use diffusion magnetic resonance imaging (MRI) to map the white matter of the brain, and magnetoencephalography (MEG) technology to map the electrical activity in the brain. “This is a very difficult problem that warrants a multimodal approach,” Roberts says. “No single modality will have the answer here. We know the delay is coming from the auditory cortex, and that’s where the MRI helps out. The source of the magnetic field can be identified in an anatomic context, so that’s the way that MRI and MEG get fused.” Roberts uses a Siemens MAGNETOM® Verio, a 3T system he credits with giving him the ability to reveal the quality of connections in the brain’s wiring. “The MRI is very good at various types of diffusion imaging,” he says. “MRI is an awesome technique.”
The second piece of technology, the MEG, allows researchers to record brain activity in real-time, in millisecond time scale. Looking something like a 1950s hair dryer, the MEG essentially measures the electrical current given off by nerve cells with every thought and feeling. “We have a helmet full of these magnetic field detectors, able to pick up spatial and temporal representation of brain function,” Roberts explains.
The Ideal Combination: Therapy and Imaging
It’s a slow process, frustratingly so for parents looking for help for their kids. But work like that being done in Philadelphia is offering glimmers of hope. And much of that hope is predicated on scanning technology.
Beyond using imaging equipment to diagnose autism earlier, systems such as MAGNETOM Verio could be used to help determine the effectiveness of behavioral and pharmaceutical therapies. Behavioral therapy “probably needs to be done hand-in-hand with imaging so we can watch brain reorganization and teach the teachers, in a sense,” Roberts says. “There are wonderful practitioners who are doing wonderful things with these children, but there’s no way to determine what is going on inside the brain, so there’s no way to tell whether what you’re doing is having an impact inside the brain or whether what you’re doing is a waste of time.” In the same way, imaging will likely play an important role in clinical trials of autism drugs, both determining their effectiveness more quickly, and screening patients to find those who are most likely to benefit.
Roberts predicts that several kinds of drug treatments for autism will be available in the next 10 to 15 years, and imaging likely will be used to help determine which drugs will help which patients. For now, he says, “Parents need to recognize signs of atypical behavior earlier. There are signs that could be picked up as early as nine to 12 months.” One common trait is a child not turning his head when a parent calls his name. “Most children respond to their name being called,” Roberts says, adding that oftentimes, parents can tell from videos of one-year birthday parties if the child isn’t interacting with other children. “If you have an early suspicion, then you should have more thorough testing and have the diagnosis confirmed,” Roberts urges, “while the brain is still more able to adapt.”
Text: Ron French
Photos: Scott Lewis
This article is part of the magazine for healthcare leadership Medical Solutions. To read more articles from this magazine visit www.siemens.com/medical-solutions
09.08.2013