Controlling antimicrobial resistance
There is no other way: We need a comprehensive approach, with everyone living up to their responsibility to combat this serious health threat in their respective areas. The most basic instinct of every living organism is survival. What selects one organism or species over another, in fact, is its capacity to withstand any kind of adverse condition that comes its way – what scientist Herbert Spencer called ‘the survival of the fittest’.
When antibiotics were invented in the early 20th century the world breathed a collective sigh of relief, thinking that the fight against infectious disease had finally been won. However, the relentless misuse and abuse of antibiotics, both in human and veterinary medicine, led to the emergence of resistant bacterial strains which, compounded with the paucity of new antibiotic molecules in the pipeline, is contributing to the desperate state-of-affairs we have today. Bacteria acquire resistance to anti-microbial agents either by mutation during replication or by encoding a mechanism of resistance from other bacteria. Microbes can easily acquire resistance to many antibiotics resulting in multi-drug resistance; in extreme cases, this can extend to all anti-microbials available on the market.
Every year in the European Union, about 400,000 citizens acquire an infection with a resistant bacterial strain and of these 25,000 die as a result. Multi-drug resistant strains infect 5-12% of hospitalised patients, especially the most vulnerable ones, such as organ transplant patients, those on haemodialysis and patients with various cancers or other chronic diseases.
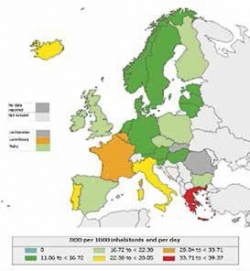
In the past four years, in more than a third of EU/EEA countries, there has been a significant increase in the trend towards combined resistance to both Klebsiella pneumoniae and E. Coli; on a more positive note methicillin- resistant Staphylococcus aureus (MRSA) has shown a decrease or stabilisation in most European countries. ECDC data from the European Surveillance of Antimicrobial Consumption Network (ESAC-Net) also showed that consumption of carbapenems increased significantly between 2007 and 2010. Iceland, Latvia and the United Kingdom have increased its antibiotic consumption by more than 5% between 2009 and 2010, while consumption fell in three other countries – Austria, Lithuania and Poland – during the same period. The vast majority of human consumption of antibiotics, in fact, occurs in the community with penicillins the most common antibiotics used.
The resistance of some microbes, notably Klebsiella and E. Coli, to a multitude of commonly used antibiotics requires the use of last line antibiotics, such as carbapenems; this places a burden on healthcare systems resulting in increasing healthcare costs, extra length of hospital stay, treatment failures and sometimes death.
The European Commission launched a 12-key action plan in November 2011 focusing on many sectors, including human and veterinary medicine. The aim is to instil and reinforce good practice over a period of five years, while introducing rigorous measures to prevent further spread of resistance. In the meantime 26 member states have implemented actions to prevent and control healthcare associated infections (HAI). The Commission has also devoted €1 billion into AMR-related research including drug projects to use existing antimicrobials in a more efficient way and to develop new molecules on the market. The Commission is also working on increased surveillance both in food safety and the transmission of resistance between animals and humans. Executive agencies like ECDC, EMA and EFSA are supporting this initiative.
Antimicrobial resistance is a responsibility of each and every one of us, be it a patient, healthcare professional or policy maker. Director General of DG Sanco, Paola Testori Coggi was very clear in her statement when she said: ‘In order to successfully address antimicrobial resistance, we need to tackle the problem in a comprehensive approach, in which all relevant parties and stakeholders live up to their responsibility to combat this serious health threat in their respective areas.’ There is no other way.
14.01.2013






