High hopes for elastography
A leading UK radiologist has highlighted how elastography has an important part to play in the future of breast imaging
Dr Bill Svensson believes that elastography has the potential to improve diagnosis of breast cancer, reduce the number of false positives in the detection of the condition and also lead to fewer biopsies performed as accuracy of imaging improves further. This June he highlighted the potential of elastography and the developments in the imaging modality at two sessions at the United Kingdom Radiology Congress (UKRC) held in Manchester, England.
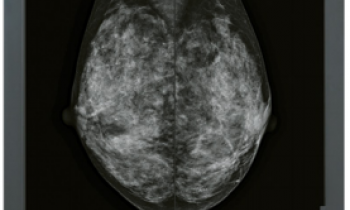
Elastography measures stiffness or strain images of soft tissue to detect or classify tumours, with a cancerous growth between five and 28 times stiffer than the background of normal soft tissue. With compression, the tumour deforms less than surrounding tissue, indicating a cancerous growth may be present.
In recent years, elastography has proved an increasingly successful tool in detection of breast cancers, primarily because of the suitability of the breast to the modality.
However, Dr Svensson remains concerned that the variability from different manufacturers in the methods available for the technique and variations in readings and colour scales, which radiologists are having to be aware of and compensate for as they take advantage of the benefits that elastography offers as a non-invasive form of diagnosis.
Dr Svensson, Reader in Breast Imaging at Imperial College London and Consultant Radiologist and Nuclear Medicine Consultant at Charing Cross Hospital, said: ‘If you add elastography into your routine work, the way in which the information is applied does not necessarily transfer directly from one manufacturer to the next.’
Siemens, for example, looks at the footprint from the stiffness strain image and the b-mode image, whereas Hitachi uses the Ueno (or variations of) pattern scoring method, said Dr Svensson. He believes it may be some years before uniformity between manufacturers is achieved. ‘The basic idea of tissue stiffness imaging is sound. The problem is the way in which tissue deforms depends on the way in which you apply a force and there are a number of ways of applying a force to get that information. It makes elastography imaging quite complex but, if you understand the physics of the machine that you are using, then you will get better results.’
He said that, in breast imaging, elastography was allowing radiologists to detect stiffer and harder areas and is a more sensitive method of imaging. ‘The ultrasound looks at those areas that deform more and those which deform less. Since we know that cancer is much stiffer than benign lesions in general and most lesions are stiffer than the fat within the breast, what elastography does is allow us to identify the stiffness.’
Advantages for the radiologist are that it provides more certainty in the image viewed and indicates what you should be getting from a biopsy result, he said, adding: ‘There are potential advantages for the patient in that it will reduce the number of needle tests that we need to do, particularly when you are doing a screening examinations. If you pick up things that you are worried about, we can use elastography to downgrade the BIRADS score.
‘Elastography may also inform the radiologist that the cancer is much more extensive than it looks on the b-mode, so that will raise the question as to whether a local excision needs to be increased or whether you need to be considering mastectomy. It will help determine the treatment.’
Dr Svensson also reflected on nine years of clinical experience with breast elastography and the major developments over that period. ‘We have seen an increase in the quality of the imaging and the ease of acquiring the elastographic data so it has become somewhat easier to interpret and understand.’
From basic strain imaging, elastography has evolved to utilise ShearWave and ARFI (acoustic radiation force impulse) imaging - a form of high energy ultrasound - to provide a more accurate way of estimating the stiffness of the tissue being examined.
Dr Svensson believes that breast elastography has tremendous potential and that in future it may be a combination of approaches that will provide better data rather than one single approach. ‘The breast has been a good place to start in terms of elastography, because it is easy to get at from an ultrasound viewpoint,’ he said, adding: ‘Breast ultrasound is also bedevilled by a very high false positive rate but elastography has the potential to reduce that.’
Dr Svensson also outlined other ways new ways of using ultrasound in the breast during UKRC, including whole breast ultrasound, using automated breast volume ultrasound (ABVS) for dense breasts and women who carry the BRCA gene associated with a high incidence of breast cancer.
Report: Mark Nicholls
15.06.2011